Justice Department Probing UnitedHealth/Optum Over Antitrust Concerns; Local Layoffs Enacted, More Forecast
Opinion Advocates for ideas and draws conclusions based on the author/producer’s interpretation of facts and data.
This is the 13th installment in an ongoing investigative series, launched in December 2022, about CareMount/Optum, broader local healthcare issues and corporate medicine.
By Adam Stone
Although I’ve done a ton of reporting over the past 14 months about Optum, and the destructive impact of the company’s takeover of our local healthcare, I haven’t previously interviewed anyone on the inside possessing internal knowledge of corporate administration.
That changed last week when I spoke to an anonymous source with intimate insight into the company’s thinking.
On Thursday, both that source and a veteran CareMount/Optum Tri-State doctor I’ve previously interviewed reached out to alert me of a new five-alarm fire: significant local layoffs were enacted last week.
I’ll get to those unfolding details in a moment, but I also have a scoop to share with potentially broader, more national implications, confirmed through internal company correspondence I obtained just days ago.
I learned last week that UnitedHealth Group, Optum’s publicly traded corporate parent, received notice on Oct. 10, 2023, that the Department of Justice (DOJ) had launched a “non-public antitrust investigation into the company,” according to a message distributed on Oct. 24 by Rupert Bondy, an executive vice president and chief legal officer of UnitedHealth Group.
Bondy’s e-mail, sent to high-ranking colleagues, concedes the disconcerting and potentially significant nature of the executives receiving a “document preservation notice” from federal law enforcement, acknowledging the “breadth of the notice” issued by U.S. authorities.
But he stressed in his note that the investigation remains in its early stages, and the demand for documents “does not mean that you have done anything wrong or have been identified as having problematic documents.”
On the Road Again
Sent to 16 members of the company, including legal counsel, Bondy’s message also notes how the DOJ has yet to issue any “specific allegations of wrongdoing.”
“It does not mean that your documents will ultimately be produced to the government, or that you will be deposed or interviewed,” Bondy asserts.
The department has made past stabs at reining in UnitedHealth’s ballooning industry power, unsuccessfully challenging the $487 billion international behemoth’s acquisition of Change Healthcare in 2022.
Meanwhile, Optum is currently moving toward acquiring Amedisys, a healthcare company that provides home health, hospice, palliative and high-acuity care services.
It’s a deal the DOJ has been scrutinizing, according to a filing with the U.S. Securities and Exchange Commission and published reports from last July.
“If they are stopped before they become a monopoly, then that’s great,” my administrative source said of the Minnesota-headquartered multinational conglomerate. “But they’re headed down that road.”
The attention from federal agents also comes as Emanate Health, a nonprofit group of hospitals and physicians based in the San Gabriel Valley in California, filed an antitrust lawsuit against Optum just three months ago, on Nov. 20, 2023.
Emanate Health alleges unfair practices in attempts by Optum to monopolize the local healthcare market, adversely impacting the nonprofit’s ability to compete.
Lowering the Boom

In January, my administrative source learned of the looming local layoffs, which were enacted last Thursday, the same day we spoke.
“The number that I saw back in January was about 119,” she said of the number of Optum Tri-State employees included on the job cuts list. “And those included some doctors, nurses, finance people, administration, administrators.”
She estimated that of the laid-off employees last week, “a solid 25 percent” come from CareMount.
Around here, the facility we previously called CareMount Medical (and MKMG/Mount Kisco Medical Group before that and established in 1946) became part of Optum Tri-State in 2022, bringing together Riverside Medical Group, CareMount and ProHealth Care.
My local doctor source confirmed that 28 pre-certification representatives were let go last week, some by e-mail, some by a phone call.
“It’s happening two weeks before they get their yearly bonus, and their yearly meeting to increase their hourly wage,” the doctor told me through an intermediary.
Outsourcing
Late last year, I also reported on the outsourcing of pre-certification work to an Indian firm, IKS.
This past weekend, I obtained company correspondence with related information, shedding additional light on the changes.
CareMount’s longtime Chief Revenue Officer, Susan Monaco, and Optum Tri-State Vice President of Revenue Cycle Info Solutions, Regina Dimayacyac, co-signed a message sent last Friday afternoon to physicians and advanced practice clinicians noting how the company had transitioned pre-authorization “to a service line team-based model.”
“To further support this transition, we have expanded our partnership with IKS to assist with our eligibility and precert functions,” they wrote in a portion of the email, framing the move as one that would “enhance our capabilities and better align our regional resources with the needs of our patients.”
‘Losing Money’
My source said planned job cuts were significant enough in volume to trigger the Worker Adjustment and Retraining Notification Act, a labor law known as WARN compliance, a factor in internal deliberations. (Post-publication note: I did not see any WARN documentation myself).
It mandates businesses with 50 or more employees to give 90 days’ notice prior for plant closings, mass layoffs, relocations or reductions in work hours, with potential penalties for non-compliance.
“So literally, as we are speaking right now, people have been let go throughout the day, all day today,” my administrative source told me in a phone interview last week, requesting anonymity for fear of reprisal.
Within the organization, staff are “freaking out,” another local source noted, also revealing that talks about unionization are now underway among beleaguered staff.
Another illuminating fact referenced by my new administrative source involved the details of Optum Tri-State’s finances.
In short, they’re not good.
Despite being owned by UnitedHealth, one of the richest companies in the world, the local unit has become an economic drain.
“Back during the summertime is when they really knew that we were losing money and not making a profit,” the insider explained about Optum Tri-State. “And then come November, they realized that, okay, we’re still not making a profit, we’re still losing money. Come fourth quarter, we’re still losing money, hence we need to figure out where we can cut and what is working and what’s not working.”
‘Give Patients Ten Minutes’
Acquiring CareMount, Riverside, ProHealth (and Crystal Run Healthcare, another lower Hudson Valley group) has proven problematic for Optum so far.
“They took on too much too fast, and they didn’t get it organized,” my administrative insider observed.
That said, the plan appears to be to enact further layoffs throughout this year, achieve profitability and eventually fold Optum Tri-State into the broader Optum East organization up and down the U.S. coast, my source explained.
“It’s going to be quite large,” the administrator added, referring to Optum East, which already has a significant grip of the eastern seaboard of the United States, in addition to its nationwide operations.
(The company’s insidious footprint is already sprawling, with about 310,000 employees around the globe; UnitedHealth Group employs or affiliates with around 90,000-plus doctors, constituting a mind-bending estimate of nearly 10 percent of all U.S. physicians.)
The administrative source also confirmed patient concerns about economic pressures forcing doctors to spend insufficient time with each patient.
“So instead of giving each patient 20 minutes, you give patients 10 minutes,” the source said of the company’s approach. “So they want doctors to see more patients in one day. So instead of seeing 25 patients in a day, they want you to see 50 patients in a day.”
Sour Note
The source wanted to be sure readers understood the significance of the players involved in last week’s regional layoffs.
People like Amit Mody, chief operating officer at Optum New Jersey, and Nicholas Korchinski, the New York chief, were among the personnel casualties, my source said.
“So it’s not just, oh, we’re going to let people in accounting go,” the administrator added. “These are people that have played significant roles in these companies.”
As top local brass started to announce departures in recent months, many observers inside the company suspected a hammer was about to drop.
“I saw the writing on the wall,” my source told me. “Basically, nobody is left in the C-suite at the Chappaqua office.”
(We reported last month on Optum Tri-State CEO Kevin Conroy’s departure, which unfolded shortly after former president Dr. Scott Hayworth also exited the enterprise, along with other recent high-profile, unfond goodbyes.)
And how will the changes impact already dissatisfied patients and distraught staff?
“I personally believe it is going to get worse,” the administrator said.
The rotten mood inside the fractured organization soured further with last week’s developments.
One of the local managers who was laid off had been in charge of the northern satellites and worked for the group for more than three decades, starting as a nurse, eventually rising to the top of MKMG/CareMount management.
“I guess they were paying her too much,” one physician lamented when referring to his trusted longtime colleague.
Justice League
An Optum finance executive, Manu Kuppalli, had been tapped to achieve local efficiencies; he’s the go-to guy to “clean up whatever financial mess is going on,” my source said.
“Patients and employees deserve better,” the administrative source added. “Not a hit squad coming in cleaning house, so to speak. And that is what these people do.”
While the source also mentioned, unprompted, how C-suite executives have been dismayed by my coverage, I asked whether there’s been pushback on the facts or the storylines.
I wanted to confirm whether the coverage was on the right big-picture track.
I’m always genuinely eager to identify unintentional blind spots in what I’ve published.
“I think your reporting is spot on,” the source replied. “And I think you’re a lot closer to – you’re hitting some nerves. How’s that?”
That’s when the source detailed the DOJ probe.
“If America’s largest health insurer is permitted to acquire a major rival for critical health care claims technologies, it will undermine competition for health insurance and stifle innovation in the employer health insurance markets,” U.S. Attorney General Merrick Garland stated on Feb. 24, 2022, when the DOJ announced a lawsuit seeking to stop UnitedHealth’s $13 billion acquisition of Change Healthcare. “The Justice Department is committed to challenging anticompetitive mergers, particularly those at the intersection of health care and data.”
However, in September 2022, UnitedHealth secured approval from a federal district court judge to finalize the deal, and the two companies formally merged the following month.
(UnitedHealth launched the Optum subsidiary in 2011 to complement its massive health insurance operation. Optum’s trio of core businesses – OptumRx, OptumHealth and OptumInsight – center on pharmacy care solutions, health management, healthcare, data analysis and industry operational support.)
‘CareMount Bills Me Again and Again’
Earlier this month I also obtained another haul of digital documents from state Attorney General Leticia James’ office. I’d submitted a Freedom of Information Law (FOIL) request last January.

The Health Care Bureau has been reviewing a litany of complaints submitted by CareMount/Optum patients, including allegations of the company double billing people and hastily sending them into collections.
There were about two dozen new patient horror stories included in the latest 107 pages of records (available on our website). Let me quickly highlight a couple representative examples.
One person referenced recurring billing issues for 18 months. The patient’s chief grievance revolved around CareMount Medical’s monthly bills, which failed to account for prior amounts owed from past bills.
“I am seeking your help because CareMount rarely, if ever, applies whatever amount I pay to the encounters for which I am actually billed,” the patient explains to the Attorney General’s Office in a June 22, 2022, complaint. “To repeat, CareMount bills me again and again, re-listing every encounter on each successive bill, even though I have paid for the prior months’ encounters.”
More Smoke
Another complaint involved duplicate charges by CareMount Medical for a single medical visit. That one drew the direct involvement of the Health Care Bureau.
A patient was allegedly charged for a service they did not receive. They couldn’t rectify the issue with the CareMount billing department.
“Since her date of service, she has received additional bills and a notice from a collection agency,” Health Care Bureau advocate Lindsay Slater of the Attorney General’s Office stated in an Apr. 6, 2022, letter to CareMount, demanding a written response.
I asked my administrative source if the chronic billing issues are the result of neglect, incompetence or something worse.
“If somebody were to ask me, knowing what I know now, whether or not people were doing it deliberately, I’ve seen people that are very ethical, very by the book, but then I’ve also seen this side of it, too,” the source said. “So I’ve seen this manipulative, very cold side. I’m not going to lie. If somebody were to say, ‘Hey, here’s the proof, here’s what we have,’ then I wouldn’t doubt it.”
And does the source believe James will bring any action?
“To be honest with you, I don’t think she’s going to get anywhere,” the source replied. “I think the DOJ may have her hold off for a bit. I think the DOJ is going to go after UnitedHealth group.”
James’ press office has not replied to my repeated requests for comment, nor has UnitedHealth/Optum.
I did submit a request for a statement from the DOJ’s public affairs department on Monday.
“As for your inquiry, we decline to comment,” Arlen Morales of the DOJ replied.
Regarding my FOIL with the state AG’s office, more documents are expected to arrive next month.
“We estimate that, by March 6, 2024, we will be able to produce to you the next installment of responsive records,” state Assistant Attorney General Abisola Fatade confirmed for me in a Feb. 7 form email about my FOIL request.
‘Deaf Ears’
I also hear almost every day from local patients, having become something of a clearinghouse for people to share their latest concerns. One expressed frustration last week after spending more than four hours unsuccessfully attempting to secure a medical appointment at Optum.
Others take to social media with their aggravation, such as a patient who posted last week about repeated cancellations, irritated by the inability to simply see their doctor.
“I couldn’t get another appointment until May,” the patient wrote on the Nextdoor platform. “I am now going to see another doctor.”
A patient I interviewed last week expressed a certain desperation that has become more and more common in people’s voices. The 66-year-old said elderly and disabled people in the community are increasingly unnerved, voicing concerns over Optum’s accessibility issues.
A resident of Putnam Lake, the longtime CareMount patient said it’s “getting bad up here, it’s getting really bad for medical care.”
Because patients can essentially no longer access their doctor for same-day care when they get sick, and are instead dispatched to urgent care, an opportunity exists for another operator, said the source, who requested anonymity, worried about the backlash of going public.
“This is what needs to be fought,” she said of area medical treatment transitioning to an urgent care model. “Either we get a medical facility up here that’s going to be just like MKMG was before they were bought out, or, you know, something has to happen up here.”
The patient’s longtime doctor left the organization last November, and she hasn’t been able to see the recommended replacement physician despite pressing medical needs, as someone with multiple handicaps and time-sensitive issues to address.

The first appointment offered after her longtime doctor’s November exit was for March – a considerable wait time given her health issues – but the session was later canceled.
“I blew my top when I got a phone call saying, ‘Well, your appointment is being canceled and we’re pushing you out to July,’” the patient fumed. “Well, that’s not going to fly for me, and that’s not going to fly for people who have certain medical conditions that need a doctor every three months to be on schedule.”
She said she’s hoping other healthcare providers, such as Nuvance or Oak Street Health, work to fill the void in the local healthcare marketplace.
“I’ve even reached out to [Oak Street] and I’ve asked, ‘If you’re in the Bronx, why can’t you come up to Westchester?’” she said. “I’ve never gotten an answer back.”
‘Cogs in a Wheel’
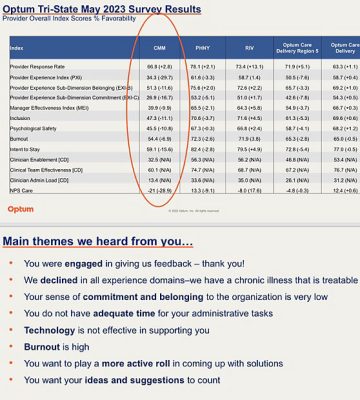
These investigative columns have uncovered the healthcare company’s oppressive physician employment contract; a disastrous phone system; urgent care upheaval; alleged double billing; copay confusion; a scathing internal survey; data privacy breaches; attorney general scrutiny; suspect COVID-19 testing charges; predatory marketing tactics; Medicare Advantage-related profiteering concerns; state lobbying efforts; a disconcerting doctor shortage; the troubling mix of healthcare with insurance services; the unethical banning of unwell patients; and the denial of patient medical records.
You also can’t overstate just how disheartened many of the top doctors and practitioners throughout the company seem to be about day-to-day decision making, sometimes of a seemingly absurd nature. My physician source recently spoke to a medical assistant who has been working for the group for more than two decades.
“She just found out on Friday that her pay raise per hour is going to be seven cents – really seven cents,” my doctor source recounted. “Are you kidding me?”
But it’s also obviously true that problems within the U.S. healthcare system stretch far beyond UnitedHealth/Optum.
Almost all physicians regularly experience burnout, with more than half considering leaving patient-facing roles or exiting the medical field entirely, amid concerns over administrative burdens, financial instability and communication demands, according to a Harris Poll conducted from Oct. 23 to Nov. 8 of last year.
Dr. John Costa, a retired local MKMG pediatrician, contacted me recently to share his deep concerns over the transformation of medical care delivery, and he prepared a guest column for The Examiner.
With more than four decades of experience – both in private practice in Bedford Hills and at MKMG through 2002 – Costa was known in his career for a commitment to community service and contributions to pediatric literature.
He attributes the broader healthcare problems to the influence of Managed Care Organizations (MCOs) and corporate interests prioritizing profit over patient care, leading to overwhelmed providers and diminished patient-doctor relationships.
Costa said policymakers need to be mindful of cumbersome regulations that make life harder for doctors. And given the current state of play, physicians should explore unionization, he also believes.
“Doctors are like cogs in a wheel,” Costa writes in his guest column. “Being told what they can and cannot do. They have lost their autonomy. They are now employees of profit-making industries. What a shame.”
He stresses how it wasn’t always like this, and it doesn’t have to be this way in the future.
Positive Vibes
As a practical matter, despite the powerful forces favoring the status quo, there does appear to be a growing, bipartisan recognition of the problems in U.S. healthcare, even if solutions remain profoundly complicated.
Examiner Editor-in-Chief Martin Wilbur and I met Congressman Mike Lawler (R-Pearl River) in December and asked him about the structural issues. He sits on the House Financial Services Committee, which maintains jurisdiction over insurance.
“I certainly have concern about insurance companies owning healthcare providers,” Lawler told us at the time. “I have real concern about how that functions and the impact that has on competition from a healthcare provider space.”
Last month I asked Lawler about a new slew of patient complaints.
“I’m deeply concerned about the reports that allege overbilling and short staffing at Optum, which provides healthcare services to so many of my constituents,” Lawler replied through spokesman Nate Soule.
Yet what matters as much, if not more, than chronicling these problems is highlighting potential solutions.
Martin and I have an interview scheduled with a relevant local stakeholder in the coming days.
I hope to report back within the next couple weeks to share related and potentially promising local healthcare news.
As always, stay tuned.
Adam Stone is publisher of Examiner Media. E-mail him with tips and feedback at astone@theexaminernews.com.

Adam has worked in the local news industry for the past two decades in Westchester County and the broader Hudson Valley. Read more from Adam’s author bio here.
